It is almost like science fiction: the ability to manipulate the human genome to cure diseases by correcting genetic errors. Since the late twentieth century, scientists have been working towards making gene therapy a reality. Gene therapy offers a chance to treat genetic diseases at their source. It involves introducing therapeutic sections of DNA into a patient’s cells, with the aim of either having that DNA translate into proteins, interfere with faulty gene expression, or even correct genetic mutations.
Typical treatment involves encoding a functional, therapeutic gene as a polymer molecule that is packaged inside a “vector” to carry the polymer into the target cells. Most of the vectors chosen are viruses, since even harmless viruses are good at infecting cells. Some viruses are even able to have their genetic material copied into the host’s cell, which scientists can exploit as a method to deliver therapeutic DNA and integrate it into the patient’s genome. Since the treatment is focused on correcting individual genetic errors, research has been focused on diseases caused by single-gene defects, such as cystic fibrosis, hemophilia, muscular dystrophy, and sickle cell anemia.
While early gene therapy research in the late twentieth century was promising, it ran into some issues in early clinical trials. Most notably, in 1999 a 19-year-old liver disease patient died during a gene therapy trial conducted at the University of Pennsylvania. The virus used as the delivery system for the therapy was from a family of viruses called Adenoviruses. Adenoviruses are infectious viruses that cause illnesses in humans such as the common cold and many other more serious diseases. The virus had its DNA stripped out and replaced with therapeutic DNA, but the patient’s immune reacted negatively to its presence. His immune system went into overdrive and attacked itself, leading to fatal organ failure. Much of the work in the field since then has gone towards matching the right virus carrier for the right disease and target area. Learning the proper dosages for therapies to be both safe and effective is also crucial.
One of the single-gene defect diseases that has been targeted recently is Usher syndrome, a rare genetic disorder that leads to gradual hearing and vision loss. It is a leading cause of deafblindness, and until now has been uncurable and largely untreatable outside of cochlear implants. The defective genes responsible for the symptoms Usher syndrome are involved with the development and maintenance of hair cells in the inner ear, called stereocilia, that send sound signals to the brain. When these hairs do not form properly due to genetic defects, they are unable to properly process sound waves, leading to deafness.
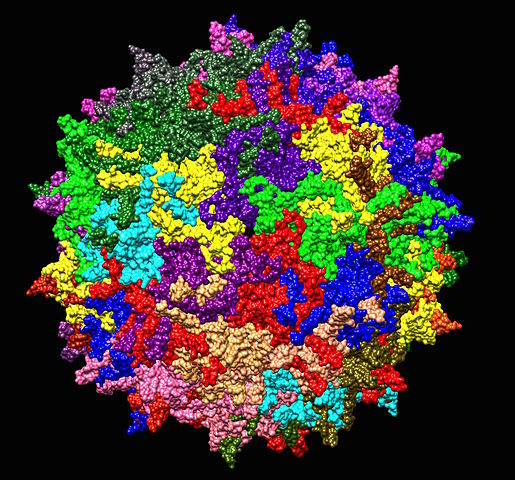
New research being done in Boston, both at Harvard and at Boston Children’s Hospital, involves using a family of viruses called Adeno-associated viruses (AAVs) as a vector for carrying therapeutic genes to treat Usher syndrome. AAVs are a class of viruses that infect humans, but unlike Adenoviruses they are not known to cause disease. This means that the patient’s immune system will usually ignore them, reducing the risk of adverse reactions. In the Boston studies, the researchers injected AAVs carrying healthy genes and protein boosters into the ears of mice with damaged inner-ear hair cells. Within 6 weeks, the mice showed signs of restored hearing – they would jump at sudden noises, which was not the case before he treatment. The mice also showed better signs of spatial awareness, which also points to restored hair cells as these are an important part of the vestibular system.
While research has advanced considerably in the last few decades, there are still many hurdles that need to be cleared before this type of treatment can be used in human. For example, the AAVs scientists are currently using are small and can’t carry very much genetic material. Treating certain forms of Usher syndrome would require carrying therapeutic genes that are much larger than can fit in the AAVs. For these larger genes to be delivered, scientists would have to come up with a new approach to get them into the target cells. They could split up the genes across multiple carriers, use a carrier with a larger capacity, or even use CRISPR/Cas-9 to edit the genes directly rather than splicing in new genetic material. Further research will investigate solving these and other problems.
For similar experiments involving mice or other rodents, Powers Scientific offers rodent chambers that are adaptable to a variety of environments. Our chambers offer a temperature and lighting-controlled environment with a temperature range of 6.5-50°C, and 0-15 fresh air exchanges per hour. Each chamber comes equipped with features such as clock-controlled lighting, solid doors, an interior outlet and access port, doors locks, an audible/visual alarm with relay, stainless steel construction, and casters. Many other options are available, including additional lighting or LED lighting, dual or multi-point temperature control for temperature stressing, top-mounted or remote compressors, extra-deep sizes, or RS-232 or data retransmit outputs. Our chambers are all built to order, allowing the individual researcher to tailor the incubator to fit the required parameters of the experiment without paying for features that aren’t needed.
For more information on our rodent incubators, see our product page, visit our contact page or call us at (800) 998-0500 and request a quote.